- Watch The JD Rucker Show every day to be truly informed.
Article originally published at American Conservative Movement and transferred here for posterity.
Update: Stanford University has disavowed the study, saying the author was no longer working for them at the time the study was conducted.
Stanford Medicine strongly supports the use of face masks to control the spread of COVID-19. pic.twitter.com/DiY3sWezCN
— Stanford Medicine (@StanfordMed) April 21, 2021
What Stanford nor any of the various fact-checkers addressing this story do not do is acknowledge that states without face mask requirements are seeing reduced Covid cases while with the strictest face masks requirements are spiking. The conclusions drawn in this study are still relevant whether Stanford and others acknowledge the scientific data or not.
Original Story:
Did you hear about the peer-reviewed study done by Stanford University that demonstrates beyond a reasonable doubt that face masks have absolutely zero chance of preventing the spread of Covid-19? No? It was posted on the the National Center for Biotechnological Information government website. The NCBI is a branch of the National Institute for Health, so one would think such a study would be widely reported by mainstream media and embraced by the “science-loving” folks in Big Tech.
Instead, a DuckDuckGo search reveals it was picked up by ZERO mainstream media outlets and Big Tech tyrants will suspend people who post it, as political strategist Steve Cortes learned the hard way when he posted a Tweet that went against the face mask narrative. The Tweet itself featured a quote and a link that prompted Twitter to suspend his account, potentially indefinitely.
Important: Our sponsors at Jase are now offering emergency preparedness subscription medications on top of the long-term storage antibiotics they offer. Use promo code “Rucker10” at checkout!
Twitter has suspended @CortesSteve for citing a Stanford NIH study about masks. pic.twitter.com/2y460zkN0Z
— Raheem. (@RaheemKassam) April 17, 2021
He was quoting directly from the NCBI publication of the study. The government website he linked to features a peer-reviewed study by Stanford University’s Baruch Vainshelboim. In it, he cited 67 scholars, doctors, scientists, and other studies to support his conclusions.
The sentence Cortes quoted from the study’s conclusion reads: “The data suggest that both medical and non-medical facemasks are ineffective to block human-to-human transmission of viral and infectious disease such SARS-CoV-2 and COVID-19, supporting against the usage of facemasks.”
Twitter messaged Cortes demanding he delete the Tweet, citing that he broke Twitter rules specifically for, “Violating the policy on spreading misleading and potentially harmful information related to COVID-19.”
Vainshelboim drew many conclusions from the vast information he compiled, but arguably the biggest bombshell in it can be found in the “Efficacy of facemasks” section [emphasis added]:
According to the current knowledge, the virus SARS-CoV-2 has a diameter of 60 nm to 140 nm [nanometers (billionth of a meter)] [16], [17], while medical and non-medical facemasks’ thread diameter ranges from 55 µm to 440 µm [micrometers (one millionth of a meter), which is more than 1000 times larger [25]. Due to the difference in sizes between SARS-CoV-2 diameter and facemasks thread diameter (the virus is 1000 times smaller), SARS-CoV-2 can easily pass through any facemask
This study isn’t the only one out there that demonstrates scientifically the inefficacy and dangers associated with constant use of face masks. One would think that considering the source, this type of information would be acceptable to even Big Tech tyrants. After all, they constantly chide us about following the science. Well, here’s the science.
Leaders in Democrat-led states should rejoice at this information since it explains why their Covid case numbers keep going up despite their ongoing lockdowns while Republican-led states are doing better. The real science gives them the answer that Dr. Anthony Fauci fails to grasp.
We’re posting the study for posterity; one never knows when the government or their puppetmasters in Silicon Valley will determine it needs to come down:
Facemasks in the COVID-19 era: A health hypothesis
Abstract
Many countries across the globe utilized medical and non-medical facemasks as non-pharmaceutical intervention for reducing the transmission and infectivity of coronavirus disease-2019 (COVID-19). Although, scientific evidence supporting facemasks’ efficacy is lacking, adverse physiological, psychological and health effects are established. Is has been hypothesized that facemasks have compromised safety and efficacy profile and should be avoided from use. The current article comprehensively summarizes scientific evidences with respect to wearing facemasks in the COVID-19 era, providing prosper information for public health and decisions making.
Introduction
Facemasks are part of non-pharmaceutical interventions providing some breathing barrier to the mouth and nose that have been utilized for reducing the transmission of respiratory pathogens [1]. Facemasks can be medical and non-medical, where two types of the medical masks primarily used by healthcare workers [1], [2]. The first type is National Institute for Occupational Safety and Health (NIOSH)-certified N95 mask, a filtering face-piece respirator, and the second type is a surgical mask [1]. The designed and intended uses of N95 and surgical masks are different in the type of protection they potentially provide. The N95s are typically composed of electret filter media and seal tightly to the face of the wearer, whereas surgical masks are generally loose fitting and may or may not contain electret-filtering media. The N95s are designed to reduce the wearer’s inhalation exposure to infectious and harmful particles from the environment such as during extermination of insects. In contrast, surgical masks are designed to provide a barrier protection against splash, spittle and other body fluids to spray from the wearer (such as surgeon) to the sterile environment (patient during operation) for reducing the risk of contamination [1].
The third type of facemasks are the non-medical cloth or fabric masks. The non-medical facemasks are made from a variety of woven and non-woven materials such as Polypropylene, Cotton, Polyester, Cellulose, Gauze and Silk. Although non-medical cloth or fabric facemasks are neither a medical device nor personal protective equipment, some standards have been developed by the French Standardization Association (AFNOR Group) to define a minimum performance for filtration and breathability capacity [2]. The current article reviews the scientific evidences with respect to safety and efficacy of wearing facemasks, describing the physiological and psychological effects and the potential long-term consequences on health.
Hypothesis
On January 30, 2020, the World Health Organization (WHO) announced a global public health emergency of severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2) causing illness of coronavirus disease-2019 (COVID-19) [3]. As of October 1, 2020, worldwide 34,166,633 cases were reported and 1,018,876 have died with virus diagnosis. Interestingly, 99% of the detected cases with SARS-CoV-2 are asymptomatic or have mild condition, which contradicts with the virus name (severe acute respiratory syndrome-coronavirus-2) [4]. Although infection fatality rate (number of death cases divided by number of reported cases) initially seems quite high 0.029 (2.9%) [4], this overestimation related to limited number of COVID-19 tests performed which biases towards higher rates. Given the fact that asymptomatic or minimally symptomatic cases is several times higher than the number of reported cases, the case fatality rate is considerably less than 1% [5]. This was confirmed by the head of National Institute of Allergy and Infectious Diseases from US stating, “the overall clinical consequences of COVID-19 are similar to those of severe seasonal influenza” [5], having a case fatality rate of approximately 0.1% [5], [6], [7], [8]. In addition, data from hospitalized patients with COVID-19 and general public indicate that the majority of deaths were among older and chronically ill individuals, supporting the possibility that the virus may exacerbates existing conditions but rarely causes death by itself [9], [10]. SARS-CoV-2 primarily affects respiratory system and can cause complications such as acute respiratory distress syndrome (ARDS), respiratory failure and death [3], [9]. It is not clear however, what the scientific and clinical basis for wearing facemasks as protective strategy, given the fact that facemasks restrict breathing, causing hypoxemia and hypercapnia and increase the risk for respiratory complications, self-contamination and exacerbation of existing chronic conditions [2], [11], [12], [13], [14].
Of note, hyperoxia or oxygen supplementation (breathing air with high partial O2 pressures that above the sea levels) has been well established as therapeutic and curative practice for variety acute and chronic conditions including respiratory complications [11], [15]. It fact, the current standard of care practice for treating hospitalized patients with COVID-19 is breathing 100% oxygen [16], [17], [18]. Although several countries mandated wearing facemask in health care settings and public areas, scientific evidences are lacking supporting their efficacy for reducing morbidity or mortality associated with infectious or viral diseases [2], [14], [19]. Therefore, it has been hypothesized: 1) the practice of wearing facemasks has compromised safety and efficacy profile, 2) Both medical and non-medical facemasks are ineffective to reduce human-to-human transmission and infectivity of SARS-CoV-2 and COVID-19, 3) Wearing facemasks has adverse physiological and psychological effects, 4) Long-term consequences of wearing facemasks on health are detrimental.
Evolution of hypothesis
Breathing Physiology
Breathing is one of the most important physiological functions to sustain life and health. Human body requires a continuous and adequate oxygen (O2) supply to all organs and cells for normal function and survival. Breathing is also an essential process for removing metabolic byproducts [carbon dioxide (CO2)] occurring during cell respiration [12], [13]. It is well established that acute significant deficit in O2 (hypoxemia) and increased levels of CO2 (hypercapnia) even for few minutes can be severely harmful and lethal, while chronic hypoxemia and hypercapnia cause health deterioration, exacerbation of existing conditions, morbidity and ultimately mortality [11], [20], [21], [22]. Emergency medicine demonstrates that 5–6 min of severe hypoxemia during cardiac arrest will cause brain death with extremely poor survival rates [20], [21], [22], [23]. On the other hand, chronic mild or moderate hypoxemia and hypercapnia such as from wearing facemasks resulting in shifting to higher contribution of anaerobic energy metabolism, decrease in pH levels and increase in cells and blood acidity, toxicity, oxidative stress, chronic inflammation, immunosuppression and health deterioration [24], [11], [12], [13].
Efficacy of facemasks
The physical properties of medical and non-medical facemasks suggest that facemasks are ineffective to block viral particles due to their difference in scales [16], [17], [25]. According to the current knowledge, the virus SARS-CoV-2 has a diameter of 60 nm to 140 nm [nanometers (billionth of a meter)] [16], [17], while medical and non-medical facemasks’ thread diameter ranges from 55 µm to 440 µm [micrometers (one millionth of a meter), which is more than 1000 times larger [25]. Due to the difference in sizes between SARS-CoV-2 diameter and facemasks thread diameter (the virus is 1000 times smaller), SARS-CoV-2 can easily pass through any facemask [25]. In addition, the efficiency filtration rate of facemasks is poor, ranging from 0.7% in non-surgical, cotton-gauze woven mask to 26% in cotton sweeter material [2]. With respect to surgical and N95 medical facemasks, the efficiency filtration rate falls to 15% and 58%, respectively when even small gap between the mask and the face exists [25].
Clinical scientific evidence challenges further the efficacy of facemasks to block human-to-human transmission or infectivity. A randomized controlled trial (RCT) of 246 participants [123 (50%) symptomatic)] who were allocated to either wearing or not wearing surgical facemask, assessing viruses transmission including coronavirus [26]. The results of this study showed that among symptomatic individuals (those with fever, cough, sore throat, runny nose ect…) there was no difference between wearing and not wearing facemask for coronavirus droplets transmission of particles of >5 µm. Among asymptomatic individuals, there was no droplets or aerosols coronavirus detected from any participant with or without the mask, suggesting that asymptomatic individuals do not transmit or infect other people [26]. This was further supported by a study on infectivity where 445 asymptomatic individuals were exposed to asymptomatic SARS-CoV-2 carrier (been positive for SARS-CoV-2) using close contact (shared quarantine space) for a median of 4 to 5 days. The study found that none of the 445 individuals was infected with SARS-CoV-2 confirmed by real-time reverse transcription polymerase [27].
A meta-analysis among health care workers found that compared to no masks, surgical mask and N95 respirators were not effective against transmission of viral infections or influenza-like illness based on six RCTs [28]. Using separate analysis of 23 observational studies, this meta-analysis found no protective effect of medical mask or N95 respirators against SARS virus [28]. A recent systematic review of 39 studies including 33,867 participants in community settings (self-report illness), found no difference between N95 respirators versus surgical masks and surgical mask versus no masks in the risk for developing influenza or influenza-like illness, suggesting their ineffectiveness of blocking viral transmissions in community settings [29].
Another meta-analysis of 44 non-RCT studies (n = 25,697 participants) examining the potential risk reduction of facemasks against SARS, middle east respiratory syndrome (MERS) and COVID-19 transmissions [30]. The meta-analysis included four specific studies on COVID-19 transmission (5,929 participants, primarily health-care workers used N95 masks). Although the overall findings showed reduced risk of virus transmission with facemasks, the analysis had severe limitations to draw conclusions. One of the four COVID-19 studies had zero infected cases in both arms, and was excluded from meta-analytic calculation. Other two COVID-19 studies had unadjusted models, and were also excluded from the overall analysis. The meta-analytic results were based on only one COVID-19, one MERS and 8 SARS studies, resulting in high selection bias of the studies and contamination of the results between different viruses. Based on four COVID-19 studies, the meta-analysis failed to demonstrate risk reduction of facemasks for COVID-19 transmission, where the authors reported that the results of meta-analysis have low certainty and are inconclusive [30].
In early publication the WHO stated that “facemasks are not required, as no evidence is available on its usefulness to protect non-sick persons” [14]. In the same publication, the WHO declared that “cloth (e.g. cotton or gauze) masks are not recommended under any circumstance” [14]. Conversely, in later publication the WHO stated that the usage of fabric-made facemasks (Polypropylene, Cotton, Polyester, Cellulose, Gauze and Silk) is a general community practice for “preventing the infected wearer transmitting the virus to others and/or to offer protection to the healthy wearer against infection (prevention)” [2]. The same publication further conflicted itself by stating that due to the lower filtration, breathability and overall performance of fabric facemasks, the usage of woven fabric mask such as cloth, and/or non-woven fabrics, should only be considered for infected persons and not for prevention practice in asymptomatic individuals [2]. The Central for Disease Control and Prevention (CDC) made similar recommendation, stating that only symptomatic persons should consider wearing facemask, while for asymptomatic individuals this practice is not recommended [31]. Consistent with the CDC, clinical scientists from Departments of Infectious Diseases and Microbiology in Australia counsel against facemasks usage for health-care workers, arguing that there is no justification for such practice while normal caring relationship between patients and medical staff could be compromised [32]. Moreover, the WHO repeatedly announced that “at present, there is no direct evidence (from studies on COVID-19) on the effectiveness face masking of healthy people in the community to prevent infection of respiratory viruses, including COVID-19”[2]. Despite these controversies, the potential harms and risks of wearing facemasks were clearly acknowledged. These including self-contamination due to hand practice or non-replaced when the mask is wet, soiled or damaged, development of facial skin lesions, irritant dermatitis or worsening acne and psychological discomfort. Vulnerable populations such as people with mental health disorders, developmental disabilities, hearing problems, those living in hot and humid environments, children and patients with respiratory conditions are at significant health risk for complications and harm [2].
Physiological effects of wearing facemasks
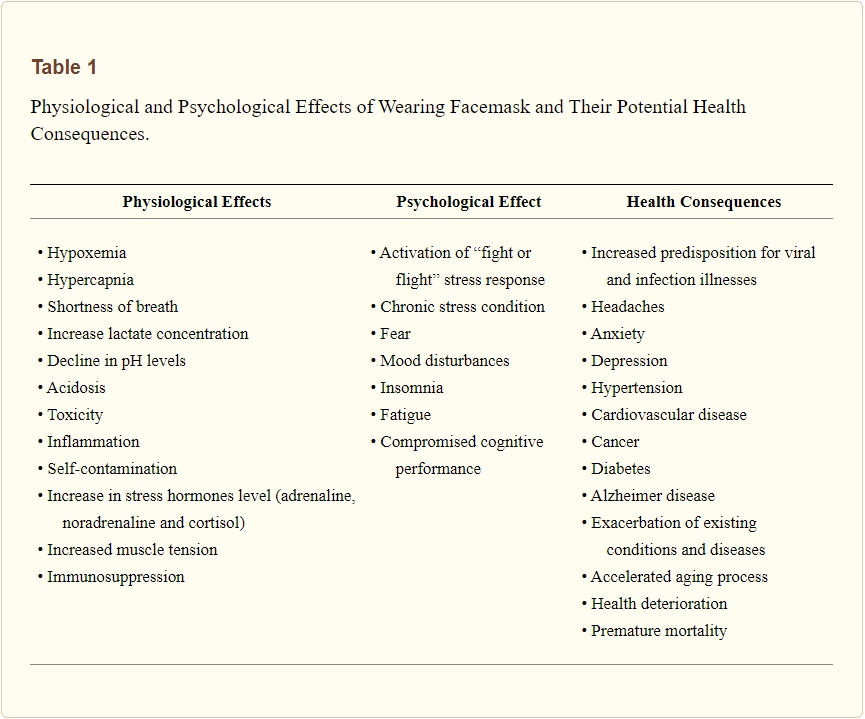
Wearing facemask mechanically restricts breathing by increasing the resistance of air movement during both inhalation and exhalation process [12], [13]. Although, intermittent (several times a week) and repetitive (10–15 breaths for 2–4 sets) increase in respiration resistance may be adaptive for strengthening respiratory muscles [33], [34], prolonged and continues effect of wearing facemask is maladaptive and could be detrimental for health [11], [12], [13]. In normal conditions at the sea level, air contains 20.93% O2 and 0.03% CO2, providing partial pressures of 100 mmHg and 40 mmHg for these gases in the arterial blood, respectively. These gas concentrations significantly altered when breathing occurs through facemask. A trapped air remaining between the mouth, nose and the facemask is rebreathed repeatedly in and out of the body, containing low O2 and high CO2 concentrations, causing hypoxemia and hypercapnia [35], [36], [11], [12], [13]. Severe hypoxemia may also provoke cardiopulmonary and neurological complications and is considered an important clinical sign in cardiopulmonary medicine [37], [38], [39], [40], [41], [42]. Low oxygen content in the arterial blood can cause myocardial ischemia, serious arrhythmias, right or left ventricular dysfunction, dizziness, hypotension, syncope and pulmonary hypertension [43]. Chronic low-grade hypoxemia and hypercapnia as result of using facemask can cause exacerbation of existing cardiopulmonary, metabolic, vascular and neurological conditions [37], [38], [39], [40], [41], [42]. Table 1 summarizes the physiological, psychological effects of wearing facemask and their potential long-term consequences for health.
Table 1. Physiological and Psychological Effects of Wearing Facemask and Their Potential Health Consequences.
In addition to hypoxia and hypercapnia, breathing through facemask residues bacterial and germs components on the inner and outside layer of the facemask. These toxic components are repeatedly rebreathed back into the body, causing self-contamination. Breathing through facemasks also increases temperature and humidity in the space between the mouth and the mask, resulting a release of toxic particles from the mask’s materials [1], [2], [19], [26], [35], [36]. A systematic literature review estimated that aerosol contamination levels of facemasks including 13 to 202,549 different viruses [1]. Rebreathing contaminated air with high bacterial and toxic particle concentrations along with low O2 and high CO2 levels continuously challenge the body homeostasis, causing self-toxicity and immunosuppression [1], [2], [19], [26], [35], [36].
A study on 39 patients with renal disease found that wearing N95 facemask during hemodialysis significantly reduced arterial partial oxygen pressure (from PaO2 101.7 to 92.7 mm Hg), increased respiratory rate (from 16.8 to 18.8 breaths/min), and increased the occurrence of chest discomfort and respiratory distress [35]. Respiratory Protection Standards from Occupational Safety and Health Administration, US Department of Labor states that breathing air with O2 concentration below 19.5% is considered oxygen-deficiency, causing physiological and health adverse effects. These include increased breathing frequency, accelerated heartrate and cognitive impairments related to thinking and coordination [36]. A chronic state of mild hypoxia and hypercapnia has been shown as primarily mechanism for developing cognitive dysfunction based on animal studies and studies in patients with chronic obstructive pulmonary disease [44].
The adverse physiological effects were confirmed in a study of 53 surgeons where surgical facemask were used during a major operation. After 60 min of facemask wearing the oxygen saturation dropped by more than 1% and heart rate increased by approximately five beats/min [45]. Another study among 158 health-care workers using protective personal equipment primarily N95 facemasks reported that 81% (128 workers) developed new headaches during their work shifts as these become mandatory due to COVID-19 outbreak. For those who used the N95 facemask greater than 4 h per day, the likelihood for developing a headache during the work shift was approximately four times higher [Odds ratio = 3.91, 95% CI (1.35–11.31) p = 0.012], while 82.2% of the N95 wearers developed the headache already within ≤10 to 50 min [46].
With respect to cloth facemask, a RCT using four weeks follow up compared the effect of cloth facemask to medical masks and to no masks on the incidence of clinical respiratory illness, influenza-like illness and laboratory-confirmed respiratory virus infections among 1607 participants from 14 hospitals [19]. The results showed that there were no difference between wearing cloth masks, medical masks and no masks for incidence of clinical respiratory illness and laboratory-confirmed respiratory virus infections. However, a large harmful effect with more than 13 times higher risk [Relative Risk = 13.25 95% CI (1.74 to 100.97) was observed for influenza-like illness among those who were wearing cloth masks [19]. The study concluded that cloth masks have significant health and safety issues including moisture retention, reuse, poor filtration and increased risk for infection, providing recommendation against the use of cloth masks [19].
Psychological effects of wearing facemasks
Psychologically, wearing facemask fundamentally has negative effects on the wearer and the nearby person. Basic human-to-human connectivity through face expression is compromised and self-identity is somewhat eliminated [47], [48], [49]. These dehumanizing movements partially delete the uniqueness and individuality of person who wearing the facemask as well as the connected person [49]. Social connections and relationships are basic human needs, which innately inherited in all people, whereas reduced human-to-human connections are associated with poor mental and physical health [50], [51]. Despite escalation in technology and globalization that would presumably foster social connections, scientific findings show that people are becoming increasingly more socially isolated, and the prevalence of loneliness is increasing in last few decades [50], [52]. Poor social connections are closely related to isolation and loneliness, considered significant health related risk factors [50], [51], [52], [53].
A meta-analysis of 91 studies of about 400,000 people showed a 13% increased morality risk among people with low compare to high contact frequency [53]. Another meta-analysis of 148 prospective studies (308,849 participants) found that poor social relationships was associated with 50% increased mortality risk. People who were socially isolated or fell lonely had 45% and 40% increased mortality risk, respectively. These findings were consistent across ages, sex, initial health status, cause of death and follow-up periods [52]. Importantly, the increased risk for mortality was found comparable to smoking and exceeding well-established risk factors such as obesity and physical inactivity [52]. An umbrella review of 40 systematic reviews including 10 meta-analyses demonstrated that compromised social relationships were associated with increased risk of all-cause mortality, depression, anxiety suicide, cancer and overall physical illness [51].
As described earlier, wearing facemasks causing hypoxic and hypercapnic state that constantly challenges the normal homeostasis, and activates “fight or flight” stress response, an important survival mechanism in the human body [11], [12], [13]. The acute stress response includes activation of nervous, endocrine, cardiovascular, and the immune systems [47], [54], [55], [56]. These include activation of the limbic part of the brain, release stress hormones (adrenalin, neuro-adrenalin and cortisol), changes in blood flow distribution (vasodilation of peripheral blood vessels and vasoconstriction of visceral blood vessels) and activation of the immune system response (secretion of macrophages and natural killer cells) [47], [48]. Encountering people who wearing facemasks activates innate stress-fear emotion, which is fundamental to all humans in danger or life threating situations, such as death or unknown, unpredictable outcome. While acute stress response (seconds to minutes) is adaptive reaction to challenges and part of the survival mechanism, chronic and prolonged state of stress-fear is maladaptive and has detrimental effects on physical and mental health. The repeatedly or continuously activated stress-fear response causes the body to operate on survival mode, having sustain increase in blood pressure, pro-inflammatory state and immunosuppression [47], [48].
Long-Term health consequences of wearing facemasks
Long-term practice of wearing facemasks has strong potential for devastating health consequences. Prolonged hypoxic-hypercapnic state compromises normal physiological and psychological balance, deteriorating health and promotes the developing and progression of existing chronic diseases [23], [38], [39], [43], [47], [48], [57], [11], [12], [13]. For instance, ischemic heart disease caused by hypoxic damage to the myocardium is the most common form of cardiovascular disease and is a number one cause of death worldwide (44% of all non-communicable diseases) with 17.9 million deaths occurred in 2016 [57]. Hypoxia also playing an important role in cancer burden [58]. Cellular hypoxia has strong mechanistic feature in promoting cancer initiation, progression, metastasis, predicting clinical outcomes and usually presents a poorer survival in patients with cancer. Most solid tumors present some degree of hypoxia, which is independent predictor of more aggressive disease, resistance to cancer therapies and poorer clinical outcomes [59], [60]. Worth note, cancer is one of the leading causes of death worldwide, with an estimate of more than 18 million new diagnosed cases and 9.6 million cancer-related deaths occurred in 2018 [61].
With respect to mental health, global estimates showing that COVID-19 will cause a catastrophe due to collateral psychological damage such as quarantine, lockdowns, unemployment, economic collapse, social isolation, violence and suicides [62], [63], [64]. Chronic stress along with hypoxic and hypercapnic conditions knocks the body out of balance, and can cause headaches, fatigue, stomach issues, muscle tension, mood disturbances, insomnia and accelerated aging [47], [48], [65], [66], [67]. This state suppressing the immune system to protect the body from viruses and bacteria, decreasing cognitive function, promoting the developing and exacerbating the major health issues including hypertension, cardiovascular disease, diabetes, cancer, Alzheimer disease, rising anxiety and depression states, causes social isolation and loneliness and increasing the risk for prematurely mortality [47], [48], [51], [56], [66].
Conclusion
The existing scientific evidences challenge the safety and efficacy of wearing facemask as preventive intervention for COVID-19. The data suggest that both medical and non-medical facemasks are ineffective to block human-to-human transmission of viral and infectious disease such SARS-CoV-2 and COVID-19, supporting against the usage of facemasks. Wearing facemasks has been demonstrated to have substantial adverse physiological and psychological effects. These include hypoxia, hypercapnia, shortness of breath, increased acidity and toxicity, activation of fear and stress response, rise in stress hormones, immunosuppression, fatigue, headaches, decline in cognitive performance, predisposition for viral and infectious illnesses, chronic stress, anxiety and depression. Long-term consequences of wearing facemask can cause health deterioration, developing and progression of chronic diseases and premature death. Governments, policy makers and health organizations should utilize prosper and scientific evidence-based approach with respect to wearing facemasks, when the latter is considered as preventive intervention for public health.
CRediT authorship contribution statement
Baruch Vainshelboim: Conceptualization, Data curation, Writing – original draft.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
[1] E.M. Fisher, J.D. Noti, W.G. Lindsley, F.M. Blachere, R.E. Shaffer
Validation and application of models to predict facemask influenza contamination in healthcare settings
Risk Anal, 34 (2014), pp. 1423-1434
[2] World Health Organization. Advice on the use of masks in the context of COVID-19. Geneva, Switzerland; 2020.
[3] C. Sohrabi, Z. Alsafi, N. O’Neill, M. Khan, A. Kerwan, A. Al-Jabir, et al.
World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19)
Int J Surg, 76 (2020), pp. 71-76
[4] Worldometer. COVID-19 CORONAVIRUS PANDEMIC. 2020.
[5] A.S. Fauci, H.C. Lane, R.R. Redfield
Covid-19 – Navigating the Uncharted
N Engl J Med, 382 (2020), pp. 1268-1269
[6] S.S. Shrestha, D.L. Swerdlow, R.H. Borse, V.S. Prabhu, L. Finelli, C.Y. Atkins, et al.
Estimating the burden of 2009 pandemic influenza A (H1N1) in the United States (April 2009-April 2010)
Clin Infect Dis, 52 (Suppl 1) (2011), pp. S75-S82
[7] W.W. Thompson, E. Weintraub, P. Dhankhar, P.Y. Cheng, L. Brammer, M.I. Meltzer, et al.
Estimates of US influenza-associated deaths made using four different methods
Influenza Other Respir Viruses, 3 (2009), pp. 37-49
[8] Centers for Disease, C., Prevention. Estimates of deaths associated with seasonal influenza — United States, 1976-2007. MMWR Morb Mortal Wkly Rep. 2010,59:1057-62.
[9] S. Richardson, J.S. Hirsch, M. Narasimhan, J.M. Crawford, T. McGinn, K.W. Davidson, et al.
Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area
JAMA (2020)
[10] J.P.A. Ioannidis, C. Axfors, D.G. Contopoulos-Ioannidis
Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters
Environ Res, 188 (2020)
[11] American College of Sports Medicine
ACSM’s Resource Manual for Guidelines for Exercise Testing and Priscription
(Sixth ed.), Lippincott Wiliams & Wilkins, Baltimore (2010)
[12] P.A. Farrell, M.J. Joyner, V.J. Caiozzo
ACSM’s Advanced Exercise Physiology
(second edition), Lippncott Williams & Wilkins, Baltimore (2012)
[13] W.L. Kenney, J.H. Wilmore, D.L. Costill
Physiology of sport and exercise
(5th ed.), Human Kinetics, Champaign, IL (2012)
[14] World Health Organization. Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak. Geneva, Switzerland; 2020.
[15] B. Sperlich, C. Zinner, A. Hauser, H.C. Holmberg, J. Wegrzyk
The Impact of Hyperoxia on Human Performance and Recovery
Sports Med, 47 (2017), pp. 429-438
[16] W.J. Wiersinga, A. Rhodes, A.C. Cheng, S.J. Peacock, H.C. Prescott
Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review
JAMA (2020)
[17] N. Zhu, D. Zhang, W. Wang, X. Li, B. Yang, J. Song, et al.
A Novel Coronavirus from Patients with Pneumonia in China, 2019
N Engl J Med, 382 (2020), pp. 727-733
[18] J.T. Poston, B.K. Patel, A.M. Davis
Management of Critically Ill Adults With COVID-19
JAMA (2020)
[19] C.R. MacIntyre, H. Seale, T.C. Dung, N.T. Hien, P.T. Nga, A.A. Chughtai, et al.
A cluster randomised trial of cloth masks compared with medical masks in healthcare workers
BMJ open, 5 (2015)
BETTER THAN DRUDGE: N.O.Q. Report is BACK as the conservative aggregator America needs.
[20] K.D. Patil, H.R. Halperin, L.B. Becker
Cardiac arrest: resuscitation and reperfusion
Circ Res, 116 (2015), pp. 2041-2049
[21] M.F. Hazinski, J.P. Nolan, J.E. Billi, B.W. Bottiger, L. Bossaert, A.R. de Caen, et al.
Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations
Circulation, 122 (2010), pp. S250-S275
[22] M.E. Kleinman, Z.D. Goldberger, T. Rea, R.A. Swor, B.J. Bobrow, E.E. Brennan, et al.
American Heart Association Focused Update on Adult Basic Life Support and Cardiopulmonary Resuscitation Quality: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care
Circulation, 137 (2018), pp. e7-e13
[23] K.G. Lurie, E.C. Nemergut, D. Yannopoulos, M. Sweeney
The Physiology of Cardiopulmonary Resuscitation
Anesth Analg, 122 (2016), pp. 767-783
[24] B. Chandrasekaran, S. Fernandes
“Exercise with facemask; Are we handling a devil’s sword?” – A physiological hypothesis
Med Hypotheses, 144 (2020)
[25] A. Konda, A. Prakash, G.A. Moss, M. Schmoldt, G.D. Grant, S. Guha
Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks
ACS Nano, 14 (2020), pp. 6339-6347
[26] N.H.L. Leung, D.K.W. Chu, E.Y.C. Shiu, K.H. Chan, J.J. McDevitt, B.J.P. Hau, et al.
Respiratory virus shedding in exhaled breath and efficacy of face masks
Nat Med, 26 (2020), pp. 676-680
[27] M. Gao, L. Yang, X. Chen, Y. Deng, S. Yang, H. Xu, et al.
A study on infectivity of asymptomatic SARS-CoV-2 carriers
Respir Med, 169 (2020)
[28] J.D. Smith, C.C. MacDougall, J. Johnstone, R.A. Copes, B. Schwartz, G.E. Garber
Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis
CMAJ, 188 (2016), pp. 567-574
[29] R. Chou, T. Dana, R. Jungbauer, C. Weeks, M.S. McDonagh
Masks for Prevention of Respiratory Virus Infections, Including SARS-CoV-2, in Health Care and Community Settings: A Living Rapid Review
Ann Intern Med (2020)
[30] D.K. Chu, E.A. Akl, S. Duda, K. Solo, S. Yaacoub, H.J. Schunemann, et al.
Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis
Lancet, 395 (2020), pp. 1973-1987
[31] Center for Disease Control and Prevention. Implementation of Mitigation Strategies for Communities with Local COVID-19 Transmission. Atlanta, Georgia; 2020.
- Concerned about your life’s savings as the multiple challenges decimate retirement accounts? You’re not alone. Find out how Genesis Precious Metals can help you secure your wealth with a proper self-directed IRA backed by physical precious metals.
[32] D. Isaacs, P. Britton, A. Howard-Jones, A. Kesson, A. Khatami, B. Marais, et al.
Do facemasks protect against COVID-19?
J Paediatr Child Health, 56 (2020), pp. 976-977
[33] P. Laveneziana, A. Albuquerque, A. Aliverti, T. Babb, E. Barreiro, M. Dres, et al.
ERS statement on respiratory muscle testing at rest and during exercise
Eur Respir J, 53 (2019)
[34] American Thoracic Society/European Respiratory, S
ATS/ERS Statement on respiratory muscle testing
Am J Respir Crit Care Med, 166 (2002), pp. 518-624
[35] T.W. Kao, K.C. Huang, Y.L. Huang, T.J. Tsai, B.S. Hsieh, M.S. Wu
The physiological impact of wearing an N95 mask during hemodialysis as a precaution against SARS in patients with end-stage renal disease
J Formos Med Assoc, 103 (2004), pp. 624-628
[36] United States Department of Labor. Occupational Safety and Health Administration. Respiratory Protection Standard, 29 CFR 1910.134; 2007.
[37] ATS/ACCP Statement on cardiopulmonary exercise testing
Am J Respir Crit Care Med, 167 (2003), pp. 211-277
[38] American College of Sports Medicine
ACSM’s guidelines for exercise testing and prescription
(9th ed.), Wolters Kluwer/Lippincott Williams & Wilkins Health, Philadelphia (2014)
[39] G.J. Balady, R. Arena, K. Sietsema, J. Myers, L. Coke, G.F. Fletcher, et al.
Clinician’s Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association
Circulation, 122 (2010), pp. 191-225
-
The Importance of Prayer: How a Christian Gold Company Stands Out by Defending Americans’ Retirement
[40] A.M. Ferrazza, D. Martolini, G. Valli, P. Palange
Cardiopulmonary exercise testing in the functional and prognostic evaluation of patients with pulmonary diseases
Respiration, 77 (2009), pp. 3-17
[41] G.F. Fletcher, P.A. Ades, P. Kligfield, R. Arena, G.J. Balady, V.A. Bittner, et al.
Exercise standards for testing and training: a scientific statement from the American Heart Association
Circulation, 128 (2013), pp. 873-934
[42] M. Guazzi, V. Adams, V. Conraads, M. Halle, A. Mezzani, L. Vanhees, et al.
EACPR/AHA Scientific Statement. Clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations
Circulation, 126 (2012), pp. 2261-2274
[43] R. Naeije, C. Dedobbeleer
Pulmonary hypertension and the right ventricle in hypoxia
Exp Physiol, 98 (2013), pp. 1247-1256
[44] G.Q. Zheng, Y. Wang, X.T. Wang
Chronic hypoxia-hypercapnia influences cognitive function: a possible new model of cognitive dysfunction in chronic obstructive pulmonary disease
Med Hypotheses, 71 (2008), pp. 111-113
[45] A. Beder, U. Buyukkocak, H. Sabuncuoglu, Z.A. Keskil, S. Keskil
Preliminary report on surgical mask induced deoxygenation during major surgery
Neurocirugia (Astur), 19 (2008), pp. 121-126
[46] J.J.Y. Ong, C. Bharatendu, Y. Goh, J.Z.Y. Tang, K.W.X. Sooi, Y.L. Tan, et al.
Headaches Associated With Personal Protective Equipment – A Cross-Sectional Study Among Frontline Healthcare Workers During COVID-19
Headache, 60 (2020), pp. 864-877
[47] N. Schneiderman, G. Ironson, S.D. Siegel
Stress and health: psychological, behavioral, and biological determinants
Annu Rev Clin Psychol, 1 (2005), pp. 607-628
[48] P.A. Thoits
Stress and health: major findings and policy implications
J Health Soc Behav, 51 (Suppl) (2010), pp. S41-S53
[49] N. Haslam
Dehumanization: an integrative review
Pers Soc Psychol Rev, 10 (2006), pp. 252-264
[50] S. Cohen
Social relationships and health
Am Psychol, 59 (2004), pp. 676-684
[51] N. Leigh-Hunt, D. Bagguley, K. Bash, V. Turner, S. Turnbull, N. Valtorta, et al.
An overview of systematic reviews on the public health consequences of social isolation and loneliness
Public Health, 152 (2017), pp. 157-171
[52] J. Holt-Lunstad, T.B. Smith, J.B. Layton
Social relationships and mortality risk: a meta-analytic review
PLoS Med, 7 (2010)
[53] E. Shor, D.J. Roelfs
Social contact frequency and all-cause mortality: a meta-analysis and meta-regression
Soc Sci Med, 128 (2015), pp. 76-86
[54] B.S. McEwen
Protective and damaging effects of stress mediators
N Engl J Med, 338 (1998), pp. 171-179
[55] B.S. McEwen
Physiology and neurobiology of stress and adaptation: central role of the brain
Physiol Rev, 87 (2007), pp. 873-904
[56] G.S. Everly, J.M. Lating
A Clinical Guide to the Treatment of the Human Stress Response
(4th ed.), NY Springer Nature, New York (2019)
[57] World Health Organization. World health statistics 2018: monitoring health for the SDGs, sustainable development goals Geneva, Switzerland; 2018.
[58] World Health Organization. World Cancer Report 2014. Lyon; 2014.
[59] J.M. Wiggins, A.B. Opoku-Acheampong, D.R. Baumfalk, D.W. Siemann, B.J. Behnke
Exercise and the Tumor Microenvironment: Potential Therapeutic Implications
Exerc Sport Sci Rev, 46 (2018), pp. 56-64
[60] K.A. Ashcraft, A.B. Warner, L.W. Jones, M.W. Dewhirst
Exercise as Adjunct Therapy in Cancer
Semin Radiat Oncol, 29 (2019), pp. 16-24
[61] F. Bray, J. Ferlay, I. Soerjomataram, R.L. Siegel, L.A. Torre, A. Jemal
Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries
CA Cancer J Clin (2018)
[62] S.K. Brooks, R.K. Webster, L.E. Smith, L. Woodland, S. Wessely, N. Greenberg, et al.
The psychological impact of quarantine and how to reduce it: rapid review of the evidence
Lancet, 395 (2020), pp. 912-920
[63] S. Galea, R.M. Merchant, N. Lurie
The Mental Health Consequences of COVID-19 and Physical Distancing: The Need for Prevention and Early Intervention
JAMA Intern Med, 180 (2020), pp. 817-818
[64] D. Izaguirre-Torres, R. Siche
Covid-19 disease will cause a global catastrophe in terms of mental health: A hypothesis
Med Hypotheses, 143 (2020)
[65] B.M. Kudielka, S. Wust
Human models in acute and chronic stress: assessing determinants of individual hypothalamus-pituitary-adrenal axis activity and reactivity
Stress, 13 (2010), pp. 1-14
[66] J.N. Morey, I.A. Boggero, A.B. Scott, S.C. Segerstrom
Current Directions in Stress and Human Immune Function
Curr Opin Psychol, 5 (2015), pp. 13-17
[67] R.M. Sapolsky, L.M. Romero, A.U. Munck
How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions
Endocr Rev, 21 (2000), pp. 55-89
Big Tech doesn’t want you to follow the science. They simply want you to follow the narrative. As Steve Cortes learned, no highly credible source is above the ugly censorship rules set by Silicon Valley tyrants.
Image by Engin Akyurt from Pixabay
Five Things New “Preppers” Forget When Getting Ready for Bad Times Ahead
The preparedness community is growing faster than it has in decades. Even during peak times such as Y2K, the economic downturn of 2008, and Covid, the vast majority of Americans made sure they had plenty of toilet paper but didn’t really stockpile anything else.
Things have changed. There’s a growing anxiety in this presidential election year that has prompted more Americans to get prepared for crazy events in the future. Some of it is being driven by fearmongers, but there are valid concerns with the economy, food supply, pharmaceuticals, the energy grid, and mass rioting that have pushed average Americans into “prepper” mode.
There are degrees of preparedness. One does not have to be a full-blown “doomsday prepper” living off-grid in a secure Montana bunker in order to be ahead of the curve. In many ways, preparedness isn’t about being able to perfectly handle every conceivable situation. It’s about being less dependent on government for as long as possible. Those who have proper “preps” will not be waiting for FEMA to distribute emergency supplies to the desperate masses.
Below are five things people new to preparedness (and sometimes even those with experience) often forget as they get ready. All five are common sense notions that do not rely on doomsday in order to be useful. It may be nice to own a tank during the apocalypse but there’s not much you can do with it until things get really crazy. The recommendations below can have places in the lives of average Americans whether doomsday comes or not.
Note: The information provided by this publication or any related communications is for informational purposes only and should not be considered as financial advice. We do not provide personalized investment, financial, or legal advice.
Secured Wealth
Whether in the bank or held in a retirement account, most Americans feel that their life’s savings is relatively secure. At least they did until the last couple of years when de-banking, geopolitical turmoil, and the threat of Central Bank Digital Currencies reared their ugly heads.
It behooves Americans to diversify their holdings. If there’s a triggering event or series of events that cripple the financial systems or devalue the U.S. Dollar, wealth can evaporate quickly. To hedge against potential turmoil, many Americans are looking in two directions: Crypto and physical precious metals.
There are huge advantages to cryptocurrencies, but there are also inherent risks because “virtual” money can become challenging to spend. Add in the push by central banks and governments to regulate or even replace cryptocurrencies with their own versions they control and the risks amplify. There’s nothing wrong with cryptocurrencies today but things can change rapidly.
As for physical precious metals, many Americans pay cash to keep plenty on hand in their safe. Rolling over or transferring retirement accounts into self-directed IRAs is also a popular option, but there are caveats. It can often take weeks or even months to get the gold and silver shipped if the owner chooses to close their account. This is why Genesis Gold Group stands out. Their relationship with the depositories allows for rapid closure and shipping, often in less than 10 days from the time the account holder makes their move. This can come in handy if things appear to be heading south.
Lots of Potable Water
One of the biggest shocks that hit new preppers is understanding how much potable water they need in order to survive. Experts claim one gallon of water per person per day is necessary. Even the most conservative estimates put it at over half-a-gallon. That means that for a family of four, they’ll need around 120 gallons of water to survive for a month if the taps turn off and the stores empty out.
Being near a fresh water source, whether it’s a river, lake, or well, is a best practice among experienced preppers. It’s necessary to have a water filter as well, even if the taps are still working. Many refuse to drink tap water even when there is no emergency. Berkey was our previous favorite but they’re under attack from regulators so the Alexapure systems are solid replacements.
For those in the city or away from fresh water sources, storage is the best option. This can be challenging because proper water storage containers take up a lot of room and are difficult to move if the need arises. For “bug in” situations, having a larger container that stores hundreds or even thousands of gallons is better than stacking 1-5 gallon containers. Unfortunately, they won’t be easily transportable and they can cost a lot to install.
Water is critical. If chaos erupts and water infrastructure is compromised, having a large backup supply can be lifesaving.
Pharmaceuticals and Medical Supplies
There are multiple threats specific to the medical supply chain. With Chinese and Indian imports accounting for over 90% of pharmaceutical ingredients in the United States, deteriorating relations could make it impossible to get the medicines and antibiotics many of us need.
Stocking up many prescription medications can be hard. Doctors generally do not like to prescribe large batches of drugs even if they are shelf-stable for extended periods of time. It is a best practice to ask your doctor if they can prescribe a larger amount. Today, some are sympathetic to concerns about pharmacies running out or becoming inaccessible. Tell them your concerns. It’s worth a shot. The worst they can do is say no.
If your doctor is unwilling to help you stock up on medicines, then Jase Medical is a good alternative. Through telehealth, they can prescribe daily meds or antibiotics that are shipped to your door. As proponents of medical freedom, they empathize with those who want to have enough medical supplies on hand in case things go wrong.
Energy Sources
The vast majority of Americans are locked into the grid. This has proven to be a massive liability when the grid goes down. Unfortunately, there are no inexpensive remedies.
Those living off-grid had to either spend a lot of money or effort (or both) to get their alternative energy sources like solar set up. For those who do not want to go so far, it’s still a best practice to have backup power sources. Diesel generators and portable solar panels are the two most popular, and while they’re not inexpensive they are not out of reach of most Americans who are concerned about being without power for extended periods of time.
Natural gas is another necessity for many, but that’s far more challenging to replace. Having alternatives for heating and cooking that can be powered if gas and electric grids go down is important. Have a backup for items that require power such as manual can openers. If you’re stuck eating canned foods for a while and all you have is an electric opener, you’ll have problems.
Don’t Forget the Protein
When most think about “prepping,” they think about their food supply. More Americans are turning to gardening and homesteading as ways to produce their own food. Others are working with local farmers and ranchers to purchase directly from the sources. This is a good idea whether doomsday comes or not, but it’s particularly important if the food supply chain is broken.
Most grocery stores have about one to two weeks worth of food, as do most American households. Grocers rely heavily on truckers to receive their ongoing shipments. In a crisis, the current process can fail. It behooves Americans for multiple reasons to localize their food purchases as much as possible.
Long-term storage is another popular option. Canned foods, MREs, and freeze dried meals are selling out quickly even as prices rise. But one component that is conspicuously absent in shelf-stable food is high-quality protein. Most survival food companies offer low quality “protein buckets” or cans of meat, but they are often barely edible.
Prepper All-Naturals offers premium cuts of steak that have been cooked sous vide and freeze dried to give them a 25-year shelf life. They offer Ribeye, NY Strip, and Tenderloin among others.
Having buckets of beans and rice is a good start, but keeping a solid supply of high-quality protein isn’t just healthier. It can help a family maintain normalcy through crises.
Prepare Without Fear
With all the challenges we face as Americans today, it can be emotionally draining. Citizens are scared and there’s nothing irrational about their concerns. Being prepared and making lifestyle changes to secure necessities can go a long way toward overcoming the fears that plague us. We should hope and pray for the best but prepare for the worst. And if the worst does come, then knowing we did what we could to be ready for it will help us face those challenges with confidence.